
As interventional radiologists, we push the boundaries of medicine with image-guided, minimally invasive treatments. Yet, pediatric IR faces hurdles that limit its impact. Awareness remains a challenge, as many referring physicians overlook pediatric IR’s potential. Training opportunities are scarce, leaving gaps in expertise. Infrastructure limitations further restrict access. By advocating for pediatric IR, expanding education, and strengthening collaboration, we can ensure more children receive life-changing care.
by Fernando Gomez
Imagen Médica, Hospital Universitario y Politécnico La Fe, Valencia, Spain
Interventional radiology has emerged as a revolutionary specialty in modern medicine. However, when it comes to pediatric patients, several significant barriers still limit access to these life-changing treatments. As interventional radiologists, it is essential to understand these challenges and advocate for solutions that make the extraordinary benefits of our therapies more accessible to children.
One of the primary obstacles we must overcome is increasing awareness of our therapeutic tools among referring physicians. Specialties such as oncology and surgery do not always consider interventional radiology as a viable treatment option, significantly reducing the chances of early intervention for certain tumors—when treatment is most effective. Additionally, many hospitals lack the necessary infrastructure to optimize pediatric care through interventional radiology. Another critical challenge is the scarcity of specialized pediatric interventional radiology training, leaving many professionals feeling unprepared to manage complex cases in children.
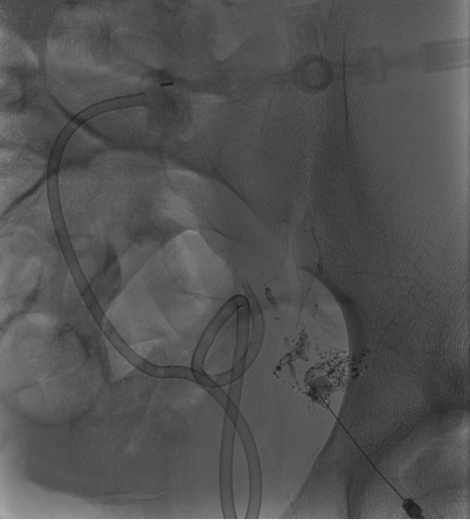
Despite these challenges, the benefits of interventional radiology for pediatric patients are immense. Treatments such as embolization, chemoembolization, sclerotherapy, percutaneous biopsies, ablation, and central line management allow us to treat numerous conditions while adhering to the principle of minimizing bodily trauma. In a fast-growing and continuously developing body, these minimally invasive techniques maximize therapeutic benefits, particularly for cancer treatment and vascular malformations.

The future of pediatric interventional radiology depends on a collective effort. It is crucial to invest in specialized training programs and advocate for all stakeholders—including healthcare ministries, patient advocacy groups, and bedside caregivers—to adapt hospital workflows and infrastructure to the needs of pediatric patients. Furthermore, educating other medical specialists about the potential of interventional radiology is essential to expanding access to these innovative treatments.
By breaking these barriers, we can ensure that more children receive cutting-edge, minimally invasive therapies—transforming not just their health but also their futures. Pediatric interventional
radiology is more than just a medical option; it is an opportunity to change lives.

Write a comment